Egg Donation
What is egg donation?
Egg donation is when a woman (a donor) goes through part of the In-vitro Fertilization (IVF) process including ovarian stimulation and egg collection procedure, in order to have some of her eggs collected. She can then donate the eggs to another woman (a recipient). The donated eggs are fertilized with the sperm of the recipient’s husband, and the resultant embryo(s) is / are transferred back into the recipient’s womb to help her conceive.
Who needs to consider egg donation?
There are many reasons why a woman might not be able to use her own eggs to conceive. Women with the following conditions may have to consider egg donation:
-
Low Ovarian Reserve or Ovarian Failure, as a result of previous chemotherapy, radiotherapy, ovarian surgery, advanced reproductive age, genetic cause or unknown cause. Women with low ovarian reserve have very small number of eggs that are usually of poor quality, resulting in IVF treatment failure. Needless to say, women who have ovarian failure cannot produce eggs at all and thus may need egg donation.
-
Poor Egg Quality, as a result of low ovarian reserve, advanced reproductive age or unknown cause. These women may have undergone IVF treatments and were found to have poor egg quality, thus leading to IVF treatment failure.
-
A Known Hereditary Disease, such as a chromosomal rearrangement or a monogenic disease. Women with these conditions may pass the genetic abnormality to their children. They can have the option of undergoing IVF and Pre-implantation Genetic Testing (PGT) to select embryos not affected by the disease for transfer. Alternatively, they can choose to use eggs from a donor who does not carry the condition so as to avoid the risk of having a child with the disease.
Is egg donation legal in Hong Kong?
Yes, egg donation is legal in Hong Kong. Like donating blood, kidney, heart and other organs, donating eggs is a gift, a voluntary act of kindness. It is ILLEGAL to buy or sell eggs in Hong Kong. A recipient cannot reward the donor for the supply of her eggs.
How to find an egg donor?
Unlike many other countries, there is no egg bank in Hong Kong that can help matching egg donors and recipients. The most commonest means for a woman to find a donor is to ask a relative or a friend to be a designated donor.
Who can be a potential egg donor?
An egg donor should be between the ages of 18 and 34 years, in good health and without any personal or family history of hereditary disease or abnormal baby. It is preferred if she has had a child of her own, but this is not essential. In addition, if the donor has donated her eggs to other women, her donation should not have resulted in more than 3 live birth events in Hong Kong.
What steps does a potential donor have to go through before she can donate her eggs?
A potential donor has to go through the following medical assessments:
-
A general body examination to make sure that she is healthy;
-
Blood tests including CBP and MCV, blood and Rhesus groups, and Pap smear test if appropriate;
-
Blood tests for Anti-Mullerian Hormone (AMH) and Follicle Stimulating Hormone (FSH) to make sure that she has a good ovarian function so that she can produce a good number of eggs after ovarian stimulation;
-
Blood tests to exclude certain infectious diseases including Hepatitis B, Hepatitis C, Syphilis, HIV and Cytomegalovirus (CMV);
-
Vaginal swabs to exclude Gonorrhoea and Chlamydia infections;
-
Blood tests for Expanded Carrier Screening (ECS) and chromosome check (karyotyping) to screen for genetic diseases.
However, infectious diseases and genetic diseases cannot be totally excluded by these investigations. Therefore, recipients need to be fully aware of this limitation before accepting egg donation.
After passing the medical assessments, the potential donor has to meet a counsellor who will discuss with her the social and psychological implications of egg donation. Then she has to see the doctor again who will discuss with her the medical procedures and risks associated with egg donation. When she is fully informed and is comfortable about donating her eggs, she can then sign the consent forms.
What steps does a potential recipient couple have to go through before they can receive egg donation?
A potential recipient couple have to undergo screening tests to enable a safe and appropriate match with the donor and to ensure the woman’s safe passage through the treatment. The recipient couple has to be assessed by a counsellor to make sure they understand the implications of the egg donation process.
The recipient woman has to go through the following medical assessments:
-
A general body examination including a transvaginal pelvic ultrasound scan to make sure that she is healthy;
-
Blood tests including CBP and MCV, blood and Rhesus groups, and Pap smear test if appropriate;
-
Blood tests to exclude certain infectious diseases including Hepatitis B, Hepatitis C, Syphilis, HIV and Cytomegalovirus (CMV);
-
Vaginal swabs to exclude Gonorrhoea and Chlamydia infections;
-
A blood test to confirm Rubella immunity.
The recipient’s husband has to go through the following medical assessments:
-
A semen analysis;
-
Blood tests for CBP and MCV, blood and Rhesus groups;
-
Blood tests to exclude certain infectious diseases including Hepatitis B, Hepatitis C, Syphilis and HIV;
-
Optional blood tests for Expanded Carrier Screening (ECS) and chromosome check (karyotyping) to screen for genetic diseases.
How long does it take before starting the IVF treatment?
Once a suitable egg donor is identified, the medical assessments and counselling of the donor and the recipient couple can be completed in about 2-3 months. When all parties feel comfortable with the donation process, then the treatment cycle can be started.
Egg Donation Flowchart
 scroll right to see more
scroll right to see more
What does the egg donor have to do when donating her eggs?
(I) Ovarian Stimulation
In order to collect more eggs, fertility drugs are used to stimulate the ovaries. The donor takes daily hormone injections in the beginning of her cycle to boost the growth of follicles (or eggs). Another injection drug, known as an antagonist, is added in the latter part of the stimulation period to prevent the eggs from being released too soon. The donor needs ultrasound scans and blood tests to monitor the growth of the follicles. When the eggs are ready, an ovulation trigger injection is given to complete the final maturation of the eggs and egg collection can be arranged.
Egg Donor: Ovarian Stimulation
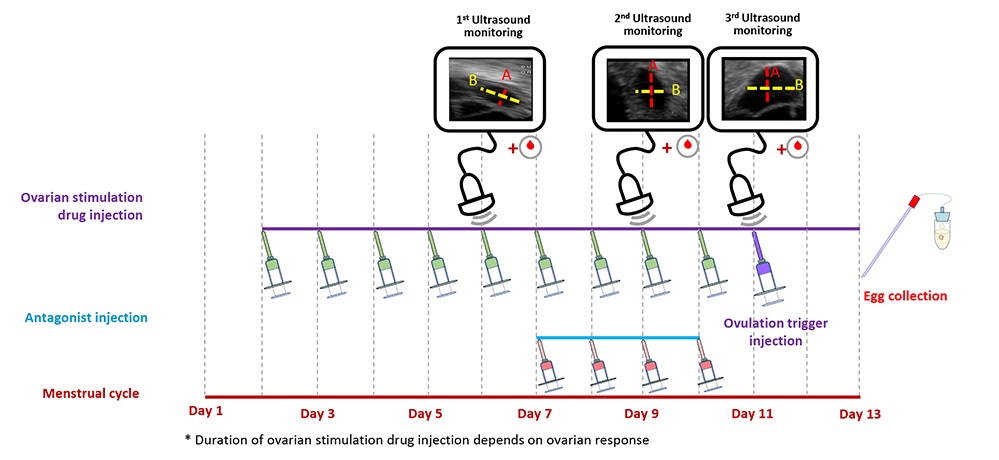
 scroll right to see more
scroll right to see more
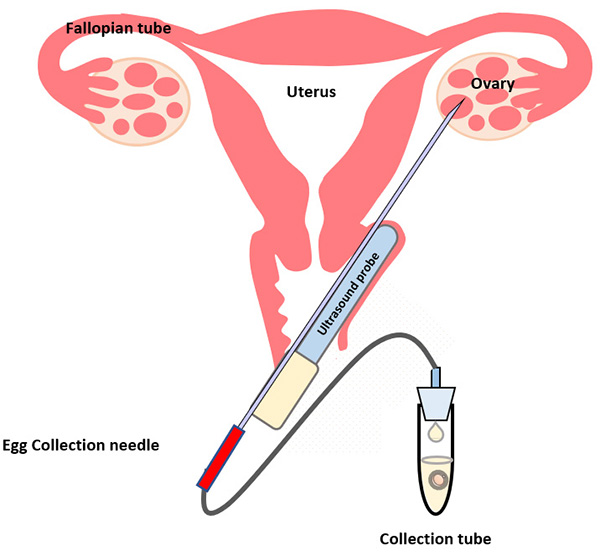
(II) Egg Collection
The egg collection procedure is performed under ultrasound guidance. An ultrasound probe is inserted into the vagina to identify the follicles. A thin needle is then inserted into an ultrasound guide to go through the vagina and into the follicles. The follicular fluid is aspirated and collected into a collection tube. An embryologist then examines the follicular fluid under a stereomicroscope to collect the eggs.
The procedure takes around 30-45 minutes. It is a painful procedure, and therefore anaesthesia is given. The woman can go home after resting in our centre for a few hours, and can return to work the next day.
 scroll right to see more
scroll right to see more
What does the egg recipient couple have to do when receiving donated eggs?
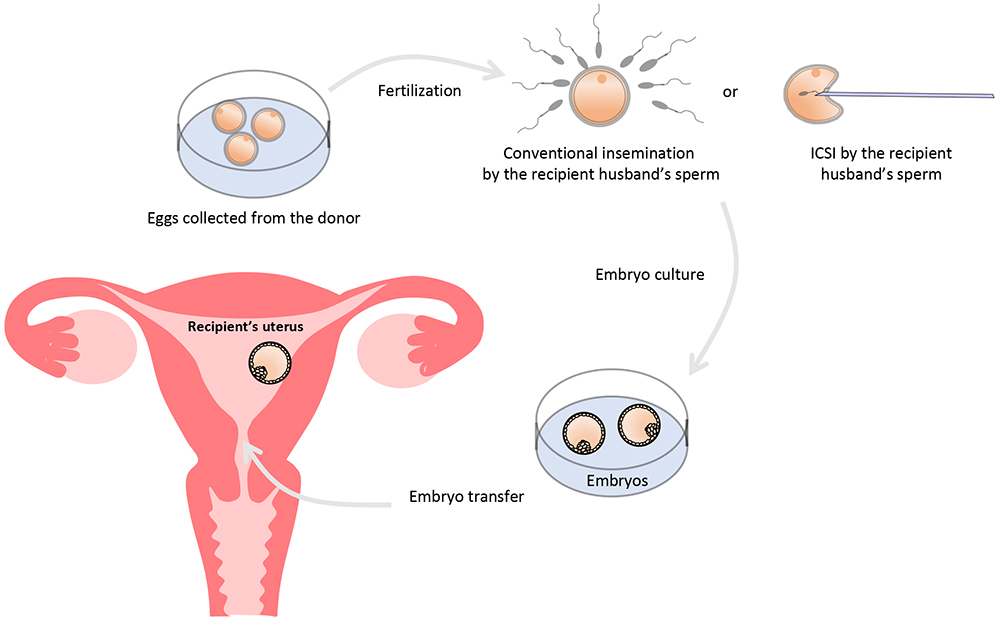
(I) Fertilization and Embryo Culture
The recipient husband has to produce a semen sample which will be used to fertilize the eggs using conventional insemination or intracytoplasmic sperm injection (ICSI). The fertilized eggs will be cultured to become embryo, which will then be transferred back into the recipient wife’s womb.
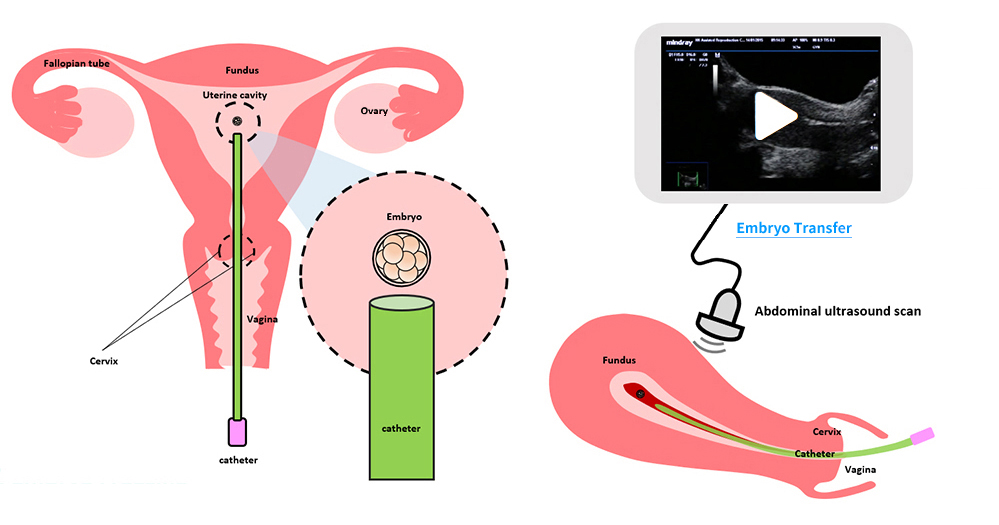
(II) Embryo Transfer
During embryo transfer, a small tube (catheter) is inserted through the cervix (the neck of the womb) and the embryo(s) is/are put into the womb cavity. The procedure is similar to taking a Pap smear. Anaesthesia or analgesia is usually not required. The recipient wife can go home after embryo transfer and resume work the next day. A pregnancy test can be done usually around 2 weeks later.
 scroll right to see more
scroll right to see more
(III) Embryo Freezing
After embryo transfer, any remaining good quality embryos are frozen for use in the future, in case treatment does not work or to try for a sibling.
How long can the embryos be stored for?
The maximum storage period for embryos produced from fertilizing donated eggs with the sperm from a designated recipient couple can be stored for up to a maximum of 2 years.