Blastocyst Culture
When are embryos transferred back to the womb?
Embryos can be transferred back to the womb at 2 different stages of their development:
-
Cleavage stage embryos on Day 2 or Day 3 of their development,
-
Blastocyst stage embryos on Day 5 of their development.
Embryo development
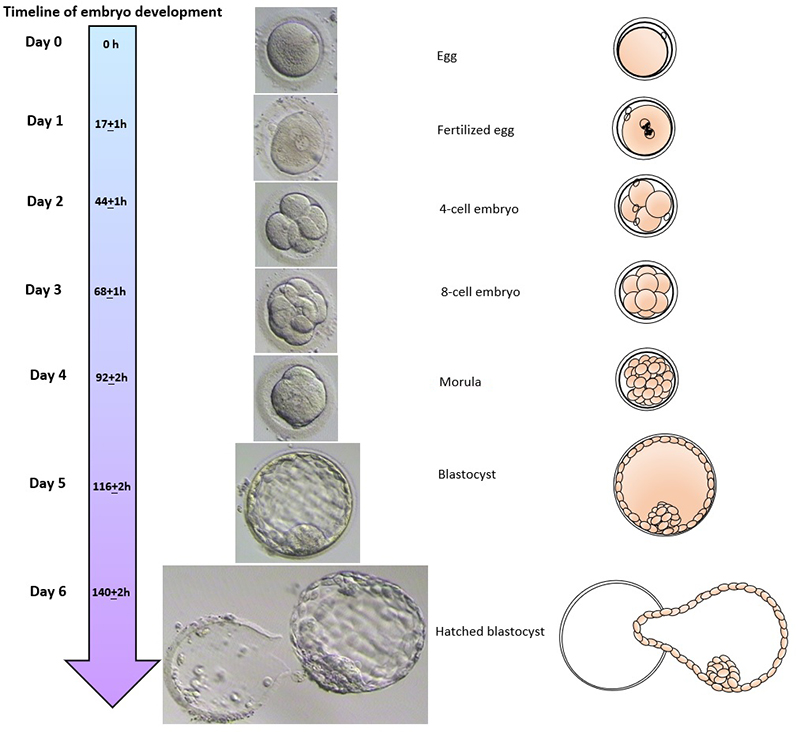
 scroll right to see more
scroll right to see more
Embryo grading
1. Cleavage stage embryos (e.g. Day 3 embryos)
A cleavage stage embryo is assessed by the number of cells in the embryo, whether the cells are even in size, and the degree of fragmentation.
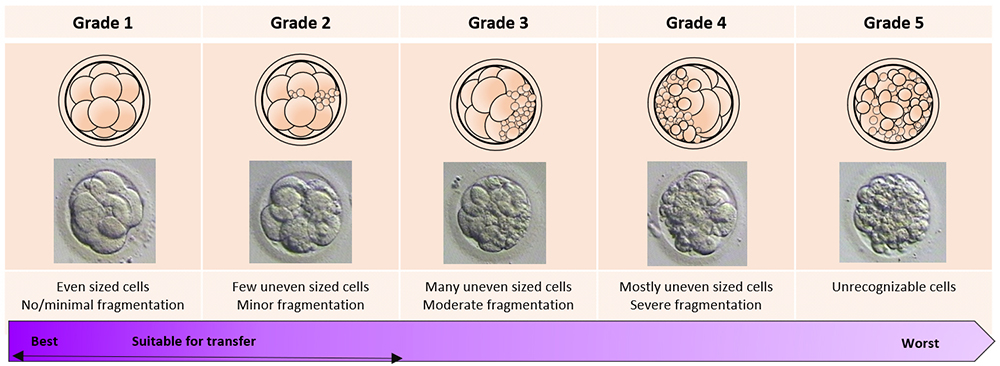
 scroll right to see more
scroll right to see more
2. Blastocyst stage embryos (e.g. Day 5 embryos)
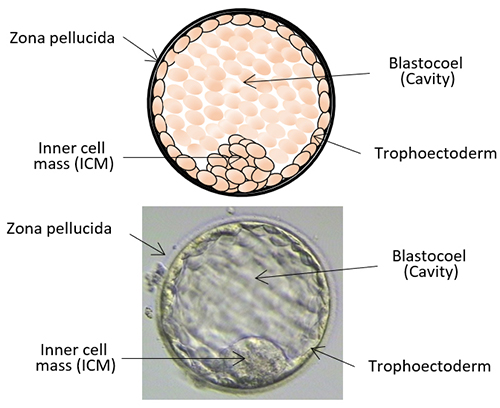
A blastocyst is assessed by the development of cavity, inner cell mass (ICM) and trophoectoderm:
-
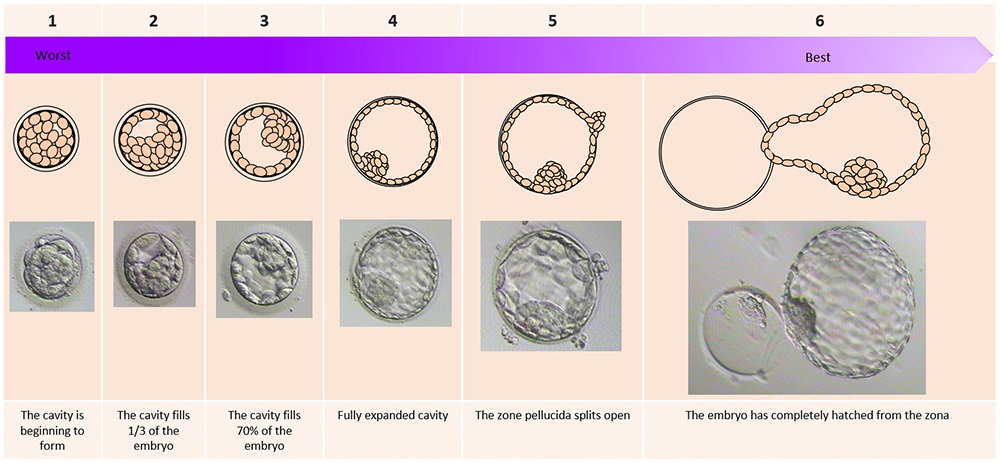
Degree of expansion of the cavity. This is graded on a scale of 1-6:
1 = the cavity is beginning to form
2 = the cavity fills 1/3 of the embryo
3 = partial expansion, the cavity fills 70% of the embryo
4 = fully expanded cavity
5 = the embryo has expanded and the zona pellucida splits open
6 = the embryo has completely hatched from the zona pellucida
-
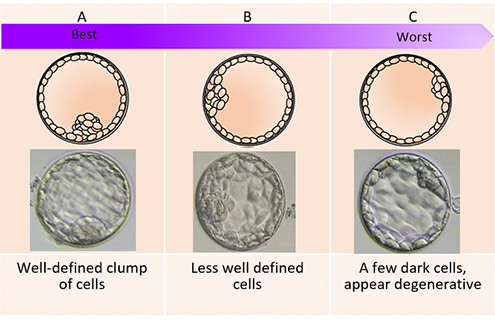
Appearance of the inner cell mass (ICM) (the cells that will grow to become the baby). This is graded into either A, B, or C:
A = well-defined clump of cells
B = less well defined; may be grainy in appearance
C = a few dark cells , appear degenerative
-
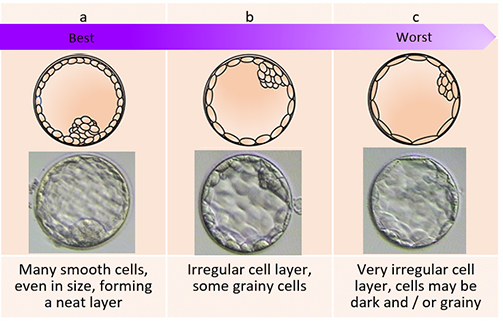
Appearance of the trophoectoderm (the cells that will form the placenta). This is also graded into either A, B or C:
A = many smooth cells, equal in size, forming a neat layer
B = irregular cell layer, some grainy cells
C = very irregular cell layer, cells may be dark and / or grainy
a. Degree of cavity expansion
 scroll right to see more
scroll right to see more
b. Inner cell mass (ICM)
c. Appearance of trophoectoderm layer
What is the difference between blastocyst and cleavage transfers?
The difference is that because blastocyst embryos have been able to develop for longer in the laboratory and they are more advance in their development, it is sometimes easier for the embryologists to select the embryos that are more likely to implant in the womb. This means that blastocyst transfer tends to have higher pregnancy rates. Statistics show that if 29% of women are pregnant with cleavage stage transfers, between 32%–42% would do so after blastocyst transfers.
What are the downsides of having blastocyst transfers?
Not all embryos that are left to the blastocyst stage will survive and some couples may have no embryo available to transfer to the womb. Even if they do, they may not have surplus embryos for freezing. This includes women who are producing very few eggs after ovarian stimulation, older women whose embryos tend to survive less well, and couples with only very few cleavage stage embryos. There is no way of knowing if the embryos had been transferred at the earlier cleavage stage, whether they could have continued to a successful pregnancy. We only know that blastocyst transfer will give you a higher pregnancy rate for each transfer attempt, but it reduces the number of total embryo transfer cycles and total number of embryos transferred as compared to cleavage transfer. It remains unclear whether the cumulative pregnancy rates after transferring all frozen embryos for each group are different.
Are multiple pregnancy rates affected by whether you have a blastocyst or cleavage transfer?
Yes, multiple pregnancy rates are higher for double blastocyst transfers compared to double cleavage transfers. Blastocyst transfer may also increase the chance of having identical twins.
Who are more suitable to have blastocyst transfers?
Generally, women who are younger, who can produce a good number of eggs after ovarian stimulation, have a good number of good quality cleavage stage embryos, and a good chance of getting pregnant, will be recommended a blastocyst transfer.